Georgia Mackenzie is an engineer that thrives in the healthcare and inclusive design landscapes. As a trained biomedical engineer, she speaks both the technical languages of the sciences as well as understanding the values and qualities of design. She is focusing on gender-inclusive design through exploring visualisations of stigmatised women’s healthcare conditions. Georgia is pursuing a master’s in Innovation Design Engineering, run by both the Royal College of Art and Imperial College London. Her bachelor’s degree is in Biomedical Engineering from the University of Virginia.
Georgia Mackenzie
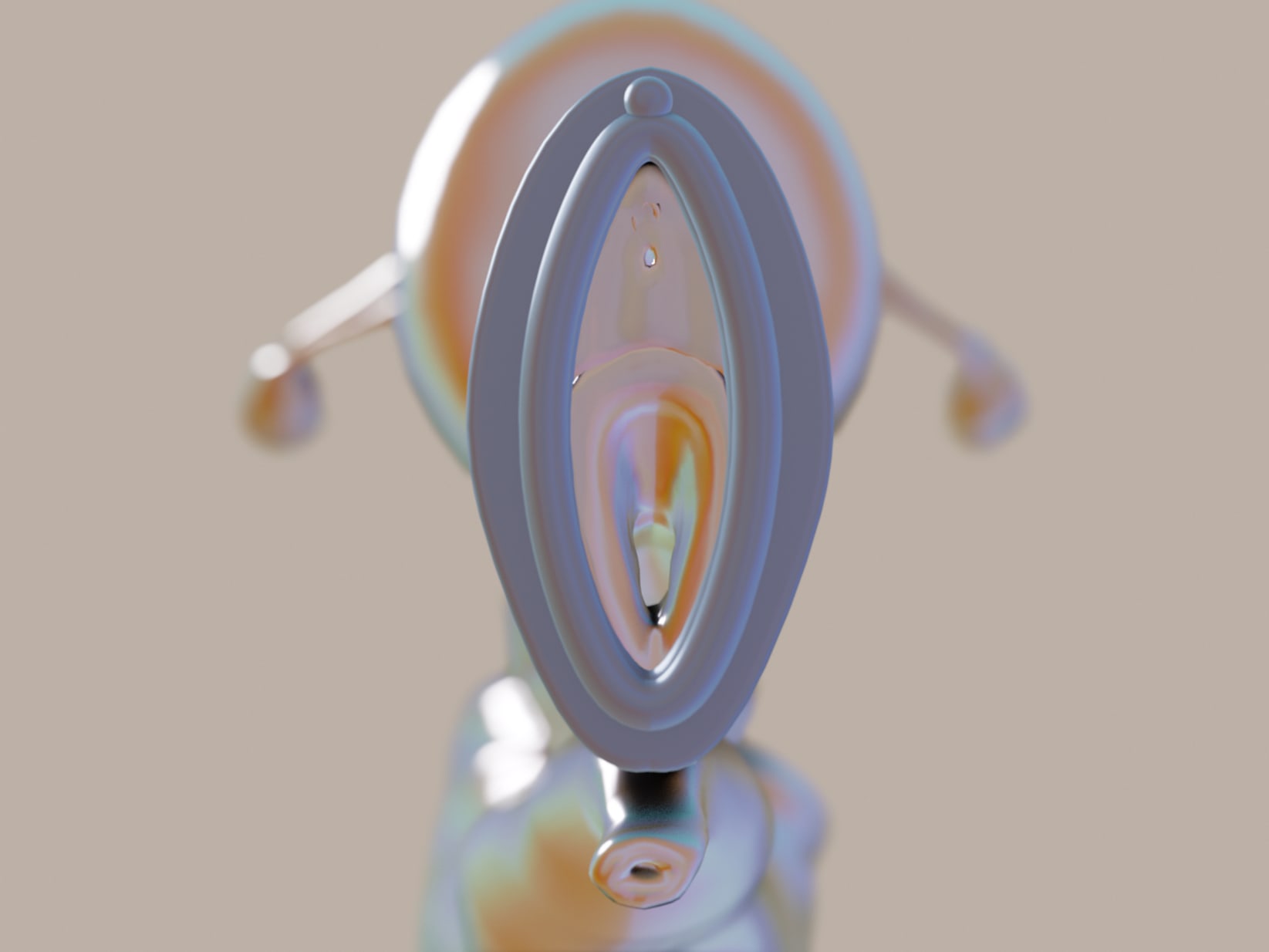

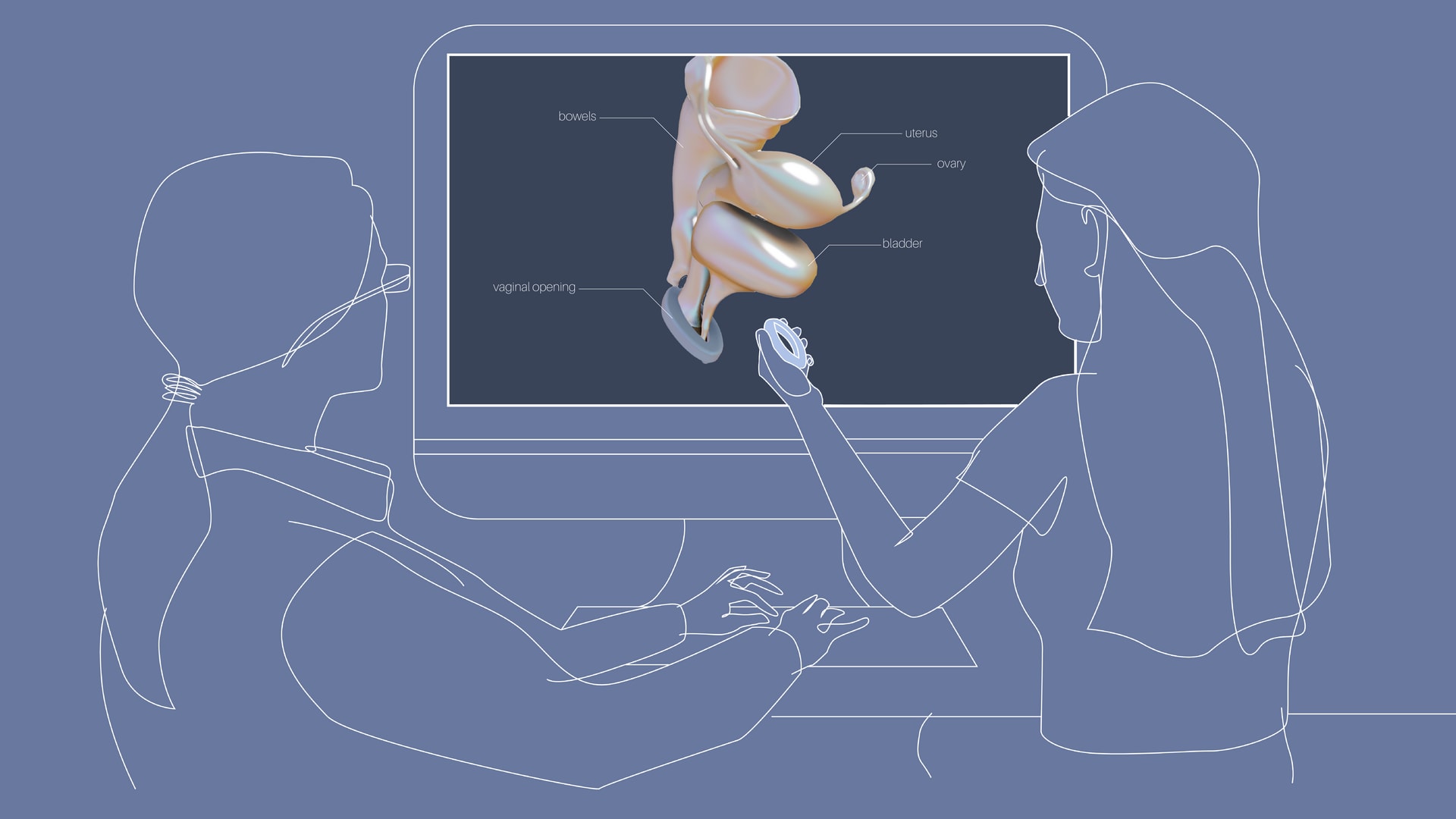
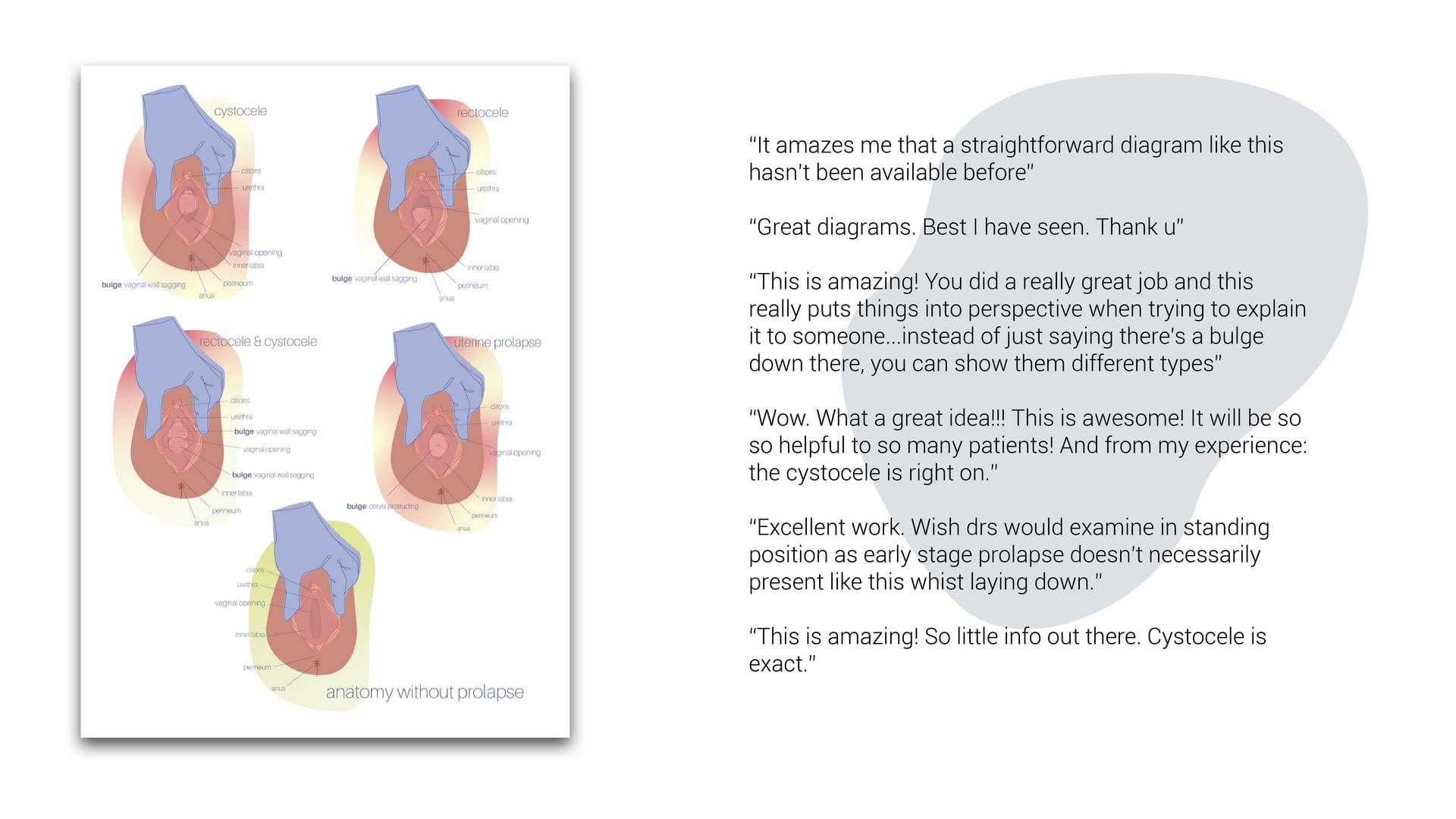
What if we took the time to listen to the stories of the silenced? 1.4 billion women worldwide have a form of Pelvic Organ Prolapse, for which there are no patient-centred diagrams and visualisations. By employing techniques of participatory design and co-design, I have collected the stories of women around the world to understand the lived experiences of prolapse, and address knowledge gaps accordingly. The result is a collection of physical and digital artefacts and illustrations, including physical conversation tools for patients, and AR overlays of internal organs.
Royal Commission of 1851
Website: https://royalcommission1851.org